Page 32 - 2016-2021-ISU
P. 32
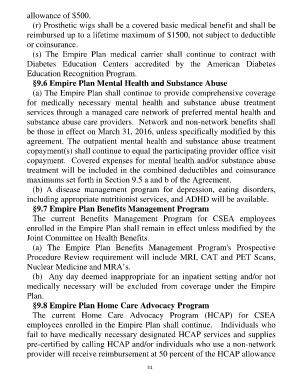
allowance of $500.
(r) Prosthetic wigs shall be a covered basic medical benefit and shall be
reimbursed up to a lifetime maximum of $1500, not subject to deductible
or coinsurance.
(s) The Empire Plan medical carrier shall continue to contract with
Diabetes Education Centers accredited by the American Diabetes
Education Recognition Program.
§9.6 Empire Plan Mental Health and Substance Abuse
(a) The Empire Plan shall continue to provide comprehensive coverage
for medically necessary mental health and substance abuse treatment
services through a managed care network of preferred mental health and
substance abuse care providers. Network and non-network benefits shall
be those in effect on March 31, 2016, unless specifically modified by this
agreement. The outpatient mental health and substance abuse treatment
copayment(s) shall continue to equal the participating provider office visit
copayment. Covered expenses for mental health and/or substance abuse
treatment will be included in the combined deductibles and coinsurance
maximums set forth in Section 9.5 a and b of the Agreement.
(b) A disease management program for depression, eating disorders,
including appropriate nutritionist services, and ADHD will be available.
§9.7 Empire Plan Benefits Management Program
The current Benefits Management Program for CSEA employees
enrolled in the Empire Plan shall remain in effect unless modified by the
Joint Committee on Health Benefits.
(a) The Empire Plan Benefits Management Program's Prospective
Procedure Review requirement will include MRI, CAT and PET Scans,
Nuclear Medicine and MRA’s.
(b) Any day deemed inappropriate for an inpatient setting and/or not
medically necessary will be excluded from coverage under the Empire
Plan.
§9.8 Empire Plan Home Care Advocacy Program
The current Home Care Advocacy Program (HCAP) for CSEA
employees enrolled in the Empire Plan shall continue. Individuals who
fail to have medically necessary designated HCAP services and supplies
pre-certified by calling HCAP and/or individuals who use a non-network
provider will receive reimbursement at 50 percent of the HCAP allowance
31